External Hemorrhoids
The condition known as piles or hemorrhoids is undoubtedly familiar to you.
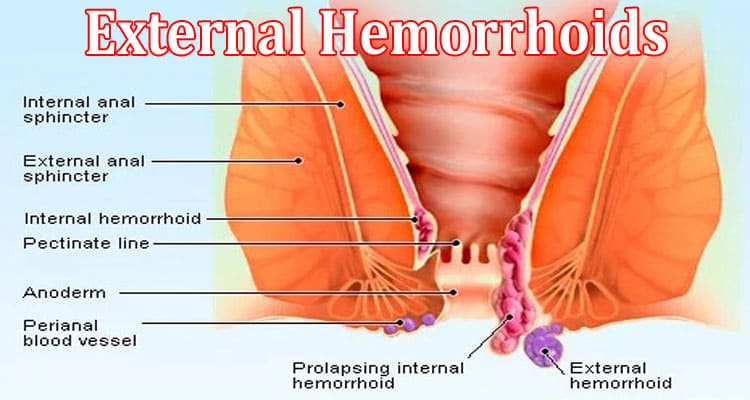
Your anus may develop lumps around inflamed veins, which can be very uncomfortable. Hemorrhoids can be internal or external, and both forms can occur simultaneously. External hemorrhoids can form beneath the skin that surrounds your anus. Internal hemorrhoids in the rectum and anus can occur.
Both types typically disappear on their own, but occasionally require medical attention.
What Causes External Hemorrhoids?
When one or more tender bumps appear beneath the skin covering your anus, you have external hemorrhoids. These are swollen, dilated blood vessels that protrude from the skin.
The blood inside the prolapsed blood vessel may thrombose, or clot. In exceptional situations, this can result in a distressing hard lump.
The origins of external and internal hemorrhoids share a lot in common. These include:
- pooping while straining– During bowel movements, repeated straining is the most frequent reason of external hemorrhoids.
- Sitting on the toilet seat for longer durations– puts pressure on the tissues around the anus and rectum.
- Pregnancy– during pregnancy there is increased pressure on the veins of the abdomen which leads to hemorrhoids.
- Obesity– obese person is at higher risk of having hemorrhoids.
- Heavy weight lifting– heavy lifting expands the risk of having hemorrhoids.
- Not consuming enough fiber– consuming dietary fiber helps to keep constipation away which will eventually avoid hemorrhoids.
- Not drinking plenty of water– drinking enough water helps to flush out excreta easily from the anus.
- Weakened support tissues– with time tissues around the area of the anus and rectum get weak.
Symptoms of External Hemorrhoids
Symptoms of external hemorrhoids are:
- Itchy anus.
- A hard lump near the anus that feels painful or tender.
- Pain and soreness in the anus, especially when sitting.
- rectal bleeding.
How to Prevent External Hemorrhoids?
Hemorrhoids are not unusual as you get older. These steps can assist save you difficult stools and constipation that may result in hemorrhoids:
- Avoid slouching or applying excessive pressure to the toilet.
- Use the restroom as soon as the desire strikes; don’t postpone bowel movements.
- When the desire strikes, use the restroom right away; don’t wait.
- Hydrate yourself well throughout the day.
- Consume more whole grains, fresh fruits, and vegetables that are high in fiber, or take supplements. In general, women should strive to consume 25 grams of fiber daily, while men should consume 35 grams.
- Continue to be active. Bowels continue to move when you’re moving.
- Only take laxatives or enemas on your doctor’s advice. It can be challenging for your body to control how you poop if you take too many laxatives or enemas.
How to Treat External Hemorrhoids at Home?
Hemorrhoids most probably go away on their own with no need of treatment. Signs like aches, discomfort, and bleeding may be one week or even longer. You can do these things in the interim to reduce symptoms:
- Apply non-prescription medications which contain Lidocaine, hydrocortisone, or witch hazel to the affected area.
- Drink plenty of water.
- Consume a high-fiber diet and supplements. Try to have of daily intake of fiber at least 20-35 grams
- Immerse in a warm bath for 10 to 20 minutes in a day.
- Take NSAIDs (nonsteroidal anti-inflammatory drugs) for burning and pain.
- Soften stool with taking laxatives.
- Use toilet paper with flushable wet wipes or lotion to mildly pat and clean up your bottom after pooping. You can also use a washcloth or tissue damped with water. (Throw away wipes in trash, exclude flushing. Clean washcloths separately by using hot water to avoid infections often found in poop.)
Medical Treatment for External Hemorrhoids
-
- Rubber band ligation- Doctors perform rubber band ligation surgery to treat internal hemorrhoids that are bleeding or prolapsing. A medical professional wraps a specific rubber band around hemorrhoid’s base. The band stops the flow of blood. Usually, within a week, the banded portion of hemorrhoid shrivels and comes off. When scar tissue develops in hemorrhoid’s residual area, it frequently contracts. This treatment should never be attempted on your own; only a doctor should perform it. Hemorrhoid frequently gets smaller because the scar tissue cuts off flow of blood.
- Infrared photocoagulation. A doctor makes use of a tool that directs infrared rays at internal hemorrhoids. The heat created by rays causes scar tissue to form, which discontinues blood supply, by shrinking hemorrhoids.
- Electrocoagulation.- Electrocoagulation. A medical professional employs a device that injects electricity into internal hemorrhoids. Hemorrhoid frequently gets smaller as a result of the electric current’s formation of scar tissue, which shuts off the blood supply.
- Hemorrhoidectomy – The total removal of the hemorrhoids is the method that works best. However, recuperation might be unpleasant and take many weeks. The doctor makes a small incision around the anus to slice them away. As it is highly sensitive near the cut, the area can be tender and painful afterward. Recovery often takes about 2 weeks, but it can take as long as 3 to 6 weeks to get normal again.
- Hemorrhoid stapling– By stopping the blood supply to internal hemorrhoids, this method pulls prolapsed tissue back into its proper position. Although recovery is simpler, there is a higher risk of the hemorrhoids returning.
Conclusion
External hemorrhoids are not life-threatening if treated on time and by maintaining a healthy lifestyle. You may need surgery if your hemorrhoid symptoms (such as bleeding, discomfort, or prolapse) persist despite medicinal treatments or office-based procedures.
Hemorrhoidectomy, which involves the surgical removal of excess hemorrhoidal tissues, is one surgical option for treating hemorrhoids. It is effective for both internal and external hemorrhoids, while other procedures, such as stapled hemorrhoidopexy and hemorrhoidal arterial ligation, are only effective for treating internal hemorrhoids. If you require surgery, your doctor can advise you on the best procedure.